A common lay term is “lazy eye.” But this is a confusing term, as it may apply to both a misaligned eye (strabismus) and / or an eye that did not develop it full visual potential due to interruption of vision development in childhood (amblyopia). The “lazy” component that refers to ocular misalignment (strabismus) can often be corrected surgically (“lazy eye surgery”) with excellent results. However the “lazy” component that refers to reduced best corrected acuity (amblyopia) generally cannot be corrected in after age 8 years. Thus “corrective surgery for lazy eye” (or “eye straightening surgery”) is generally quite effective in correcting ocular misalignment and its impact on social communication, but is generally ineffective in improving the best corrected acuity of the affected eye (amblyopia component).
Strabismus may also display “patterns”
“A” pattern –
eyes move closer to each other when looking up and further away when looking down.
“V” pattern –
eyes move away from each other when looking up and closer to each other when looking down.
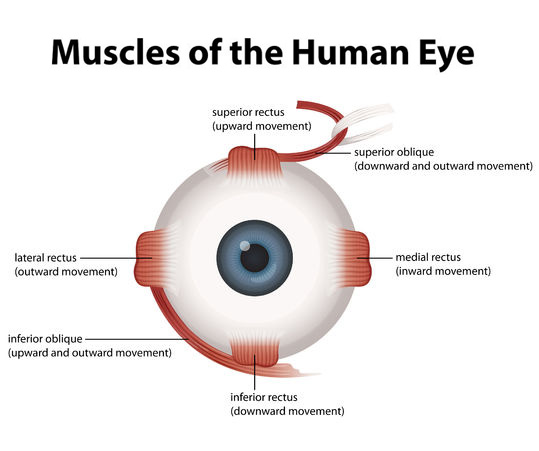
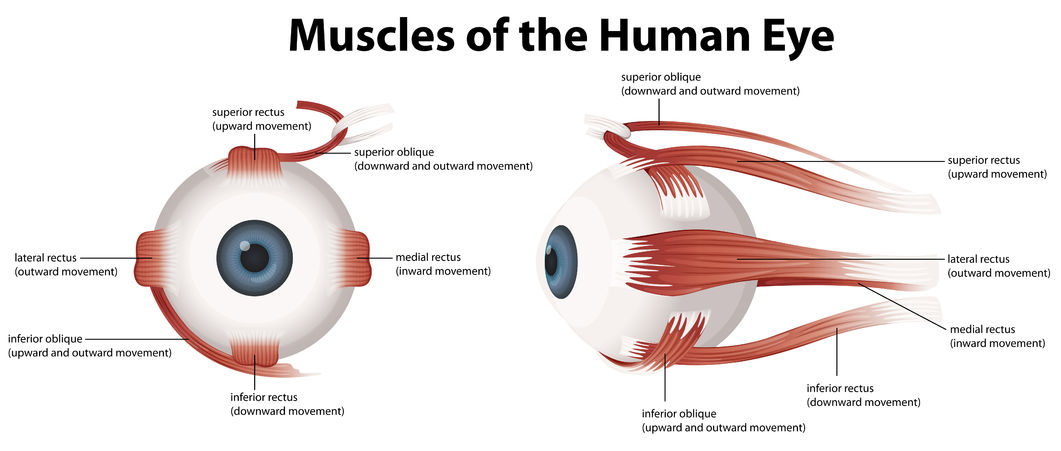
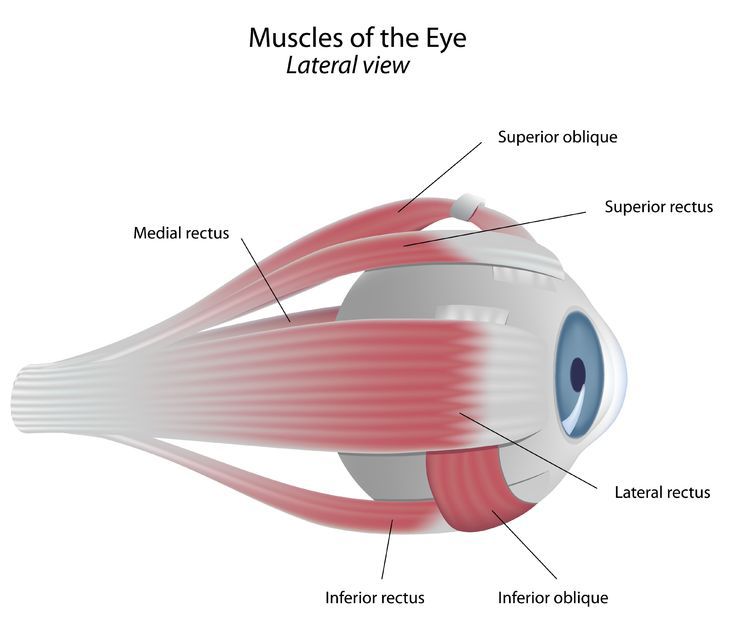
In the majority of cases the eye muscles are normal. The problem lies in the pathways that govern neurologic input to the eye muscles. Although we have an understanding of the various brainstem nuclei that innervate the eye muscles, our understanding of the complex pathways that govern eye movement is lacking. The best option available is to surgically weaken or strengthen the eye muscles. The amazing part is that is works quite well in addressing the problem: I tell patients that in my experience 90% improve 90%. Over the years, various tables have been developed that help the surgeon to determine how much to move a muscle to get a desired amount of response. Still, some patient’s don’t follow the textbook tables! Here is were adjustable sutures come into place. The eye muscle can be placed on a special kind of slip knot that allows the surgeon to adjust its position in the first 24 hours of surgery. Thus the great majority of over or under-corrections in the immediate post-operative period can be easily corrected.
Over the long term re-operations are not uncommon as some individuals experience a recurrence or over-correction (up to 20% in some studies). Exercises to improve strabismus, as supported by some vision therapists, are generally ineffective.
Strabismus in adults is often due to a recurrence of childhood correction of strabismus. In other cases, it may represent a childhood or congenital condition that has slowly deteriorated over time (e.g. decompensated congential 4th nerve palsy). As a result, the field of Pediatric Ophthalmology has evolved over time into a combined field of Pediatric Ophthalmology and Adult Strabismus.
Whenever there is acute onset of strabismus, and whenever there is incomitance (i.e. the degree of ocular deviation is Not the same in the various positions of gaze) the clinician needs to have a high suspicion for underlying serious central nervous system disorders such as a brain tumor or stroke.
When strabismus is variable (angle of deviation varies throughout the day) consideration to ocular myasthenia should be given.
Certain conditions can cause progressive fibrosis or thickening of the eye muscles. This is particularly true of thyroid-related eye disease (also known as Graves Disease).
Strabismus may also be caused by blunt trauma. Orbital fracture can entrap the eye muscles, or tissues attached to them, and cause restriction of eye movement.
In some (especially children) strabismus is due to hyperopic refractive error. These individuals, who are generally “far-sighted” experience eye crossing that is corrected by wearing glasses. Affected children often “outgrow” the condition (accommodative esotropia) with age.
There is no skin incision. An incision is generally made in the conjunctiva, which once healed is often undetectable. A special hook is place under the eye muscle, allowing an absorbable suture to be place close to the insertion of the muscle onto the eye. The muscle is detached and sewn back / secured in a new position.
The time for surgery is dependent upon the eye muscles that are moved – a reasonable estimate is about 30 minutes per eye muscle.
Some surgeons perform strabismus surgery under local or topical anesthesia. But the great majority use general anesthesia, to avoid patient discomfort and to permit a more controlled operating environment.
In the great majority of cases, surgery is done on an outpatient basis (i.e. no hospital stay) and there is not eye patch after surgery. Patient fast for 8 hours before the procedure, come to the surgery center in the morning and are back home by early afternoon. I always examine the patient the following morning. In a minority of cases (1-2%) a suture adjustment is necessary the day after surgery (please see “adjustable sutures” above)